Information
Journal Policies
Polyhydramnios in Diabetes Mellitus-Complicated Pregnancy: Severe as Never Seen Before
Piazze Juan1*, Donfrancesco Cristina1,2, Testani Costantino1
2.Department of Experimental Medicine, University of Rome “Sapienza”, Rome (RM), Italy.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Polyhydramnios is defined as an increase in the amniotic fluid over 240 mm as evaluated by the amniotic fluid index at ultrasound evaluation; the highest limit as evaluated by this ultrasound technique is difficult to set.
In this manuscript we present a case of severe polyhdramnios, in one pregnancy affected by diabetes mellitus, which reached ultrasound evaluated amniotic fluid values as never seen and described before.
Diabetes mellitus, insulin therapy, polyhydramnios, amniotic fluid index, ultrasound, neonatal hypoglycemia.
1. Introduction
Diabetes mellitus is the most frequent medical complication of pregnancy. Approximately 90% of the cases are represented by Gestational diabetes mellitus (GDM), which affects 2-5% of all pregnancies [1], while pre-existing diabetes mellitus complicates 0.2% to 0.3% of pregnancies [2].
Diabetes complicated pregnancies are at increased risk both for the foetus and the mother. There is an increased incidence of congenital malformations and perinatal morbidity [3-5], and diabetic mothers are at risk of progression of microvascular diabetic complications as well as miscarriage, pre-eclampsia, polyhydramnios and premature labour [6].
Polyhydramnios is a frequent complication linked to and altered maternal glycemic control. An increased amniotic fluid index (AFI > 240 mm) defines this situation. However, the cases of highest AFI values are not described in the literature.
The present case describes a severe polyhdramnios in one pregnancy affected by diabetes mellitus with good postnatal outcome both for the mother and the baby.
2. Case Report
A gravida 3, para 2, 41-year-old white woman at 34 weeks of pregnancy presented at our Institution for an ultrasound (US) evaluation. She was affected by diabetes mellitus from the age of 23, and 10 years after the diagnosis had developed diabetic retinopathy too. Her previous pregnancies were both complicated by macrosomia: the first baby was a female weighting 4650 gr at spontaneous birth, while the second was a female however delivered by caesarean section in consideration of the estimated weight, which was 5200 gr at birth.
Her third pregnancy was a spontaneous miscarriage occurred at 18 weeks.
She was under insulin therapy from her second pregnancy, and glycemia was always under control.
She performed all the requested analysis for this pregnancy: her glycemia resulted well controlled by insulin administration, second trimester ultrasound, fetal echocardiogram and other fetal evaluations were all within limits.
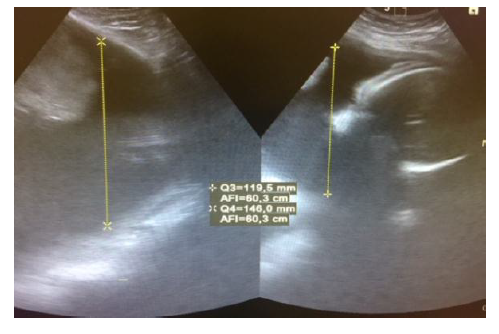
At our US evaluation at 34 weeks she presented a large for gestational age (LGA) fetus, on the 80th percentile according to Hadlock 4 curves and a severe polyhydramnios, with an AFI at 510 mm. Fetal and maternal Doppler velocimetry documented a good fetal oxygenation. She was hospitalized, in order to monitor her glycemia and to make a diabetic assessment. Her glycemia revealed not to be adequately controlled, so insulin therapy was adjusted. She was treated with rapid acting insulin three times per day (12 IU at breakfast, 16 IU at lunch and 12 IU at dinner) and 36 IU of long acting insulin in the evening. She was discharged home with a good glycemic status control. The patient was therefore evaluated every two weeks. At 38 weeks, she presented a good glycemic status control and her glycated hemoglobin (HbA1c) was 6.6% (normal 4.3-6.1%). However, at US evaluation, AFI was increased at 603 mm (Figure1), estimated fetal weight kept on the 80th percentile, fetal and maternal Doppler velocimetry were good. Four days later a cesarean section (CS) was planned.
A female child, weighting 4630 gr, was born. The baby suffered of neonatal severe hypoglycemia, but she was promptly assisted at the intensive care unit. Regarding the mother, the surgery was uneventful, the postoperative course and her blood exams were normal. The patient was discharged home three days after CS in healthy conditions, after an adjustment, i.e., a decrease of insulin therapy according to her glycemic conditions.
The baby was hospitalized for one week but then she was discharged in good health and presenting no risk conditions.
3. Conclusions
Glycemic control before and during pregnancy is essential for the good outcome of pregnancy, in order to reduce the risk of neonatal macrosomia and hypoglycaemia. Post-partum evaluation of glucose tolerance and appropriate counselling in women with GDM is relevant too, in order to decrease the subsequent risk of type 2 diabetes in the long term.
One of the most relevant element to consider in pregnancy is represented by the amniotic fluid index (AFI) at ultrasound evaluation. When it is increased it can reflect a scarce control of glycemia, leading to fetal and neonatal complications. Polyhydramnios is defined as an increase in the AFI over 240 mm (normal range 120-160 mm), but the highest value is difficult to set.
Regarding the AFI value, it was always surprising to see, even in comparison of all the experience accumulated in more than two decades of research regarding amniotic fluid dynamics [7-8].
In the present case, fetal macrosomia and the dramatically increased AFI value may reflect a not adequate maternal glycemic control. And these parameters were constant in all the successive controls even after the insulin therapy was adjusted.
The constant preoccupation for similar clinical situations are the risk of a preterm labor 9 due to the membrane stress caused by the high amniotic fluid volume and consequent compression or other cases such as an extremely high AFI in one pregnancy with a precedent cesarean section which would lead to an increased risk of imminent delivery.
References
- Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational diabetes and its association with type 2 diabetes mellitus. Diabetic Med2004; 21:103-13.
- Risk of Complications of Pregnancy in Women with Type 1 Diabetes: Nationwide Prospective Study in the Netherlands. BMJ2004; 328: 915-9.
- Outcome of pregnancy in diabetic women: more investigation is needed into whether control of diabetes is really poorer in England than Norway. BMJ2001; 322:614-5.
- TD, Mathiesen E, Ekbom P, Hellmuth E, Mandrup-Poulsen T, Damm P. Poor Pregnancy Outcome in Women with Type 2 Diabetes. Diabetes Care2005; 28:323-8.
- DM, Damm P, Moelsted-Pedersen L, Ovesen P, Westergaard JG, Moeller M, Beck-Nielsen H. Outcomes in Type 1 Diabetic Pregnancies: A nationwide, population-based study. Diabetes Care2004; 27:2819-23.
- Biesty LM, Egan AM, Dunne F, Dempsey E, Meskell P, Smith V, Ni Bhuinneain GM, Devane D. Planned birth at or near term for improving health outcomes for pregnant women with gestational diabetes and their infants. Cochrane Database Syst Rev2018 Jan 5; 1: CD012910. Doi: 10.1002/14651858. CD012910.
- Piazze JJ, Anceschi MM, Ruozzi Berretta A, Vitali S, Maranghi L, Amici F, Cosmi EV. The combination of computerized cardiotocography and amniotic fluid index for the prediction of neonatal acidemia at birth: a modified biophysical profile.J Matern Fetal Med2001; 10:323-7.
- Piazze J, Anceschi MM, Cerekja A, Brunelli R, Meloni P, Marzano S, Cosmi E. Validity of amniotic fluid index in preterm rupture of membranes.J Perinat Med2007;35:394-8.
- ManyA, Lyndon M, Lazebnik N, Martin JG. The association between polyhydramnios and preterm delivery. Obstet Gyn 1995;86:389-391.