Information
Journal Policies
CBCT Findings of Ossifying Fibroma in the Mandible: A Case Report
Nagihan Koc1*, Kubra Karakoc Guvenc2
2.Department of Periodontology, Faculty of Dentistry, Suleyman Demirel University, Cunur, 32200 Isparta, Turkey.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Fibro-osseous lesion is a generic designation for a diverse group of bone lesions that have similar histological features. The condition is characterised by the replacement of the normal bone by the fibro-osseous tissue. Ossifying fibroma is a benign fibro-osseous lesion of the maxillofacial and oral region which occurs mostly in patients between the ages of 20 to 40 years. This report describes a case of ossifying fibroma in a 37-year-old female patient with emphasis on the cone-beam computed tomographic features.
Keywords: Diagnostic Imaging; Cone-Beam Computed Tomography; Fibroma, Ossifying,Dental Science
1. Introduction
Fibro-osseous lesions of the bones comprise of a group of benign lesions that are named for the similarity in their histological appearance. They are composed of varying amounts bone or cementum-like tissue in fibrous connective tissue stroma [1]. Ossifying fibroma (OF) is a slow-growing, well-circumscribed fibro-osseous lesion of the bone that is thought to be derived from periodontal ligament [2]. OF is usually diagnosed in female patients below 40 years of age. It can occur in any cranio-facial bone but is noted to occur most often in the mandible premolar and molar regions [3,4]. Some cases of OF exhibit more aggressive behaviour. Such cases appear in younger individuals and are called juvenile OF.
Clinically, OF is asymptomatic during the early stages of its development [5]. However, the continuous expansion of the involved bone may result in pain, swelling and tooth displacement [3,4]. In certain cases, the lesion can cause obstruction of the nasal fossae or maxillary sinus, facial asymmetry, eye protrusion and neurological complications[3,6].
On imaging, OF appears as a well-defined lesion including two major patterns: expansile unilocular radiolucencies, with or without opacifications and multilocular configuration [7]. The slow but persistent growth of the tumour within the jaws may cause expansion and thinning of the cortical plates [3,8,9].
Management of the OF include curettage, enucleation, and radical resection with reconstruction of the surgery site [3-5]. This report describes a case OF in the mandible according to its cone-beam computed tomographic (CBCT) findings.
2. Case Report
A healthy 37-year-old female was referred to the radiology clinic by a local dentist for the evaluation of a well-defined lesion with multilocular radiopacities in the mandible. Her medical history was unnoticeable. Clinical examination revealed a painless swelling around the lingual aspect of the left posterior region of the mandible. The patient was unaware of the duration of the swelling. She had no history of trauma. Intra-orally, the covering mucosa and teeth were normal. The vitality of involved posterior teeth was confirmed with the electric pulp tester.
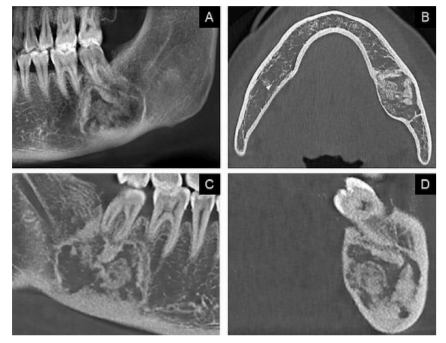
The cone-beam computed tomography (CBCT) images revealed a well-demarcated expansile lesion with a sclerotic border located at the apex of the mandibular left second molar. The interior aspect of the lesion showed a mixed radiopaque radiolucent pattern (Figure 1). The lesion was in close proximity to roots of the mandibular first and second molars. However, there were no signs of root resorption. Displacement of the inferior alveolar canal and expansion and thinning of the lingual cortical plate were observed on the sagittal and coronal CBCT images. The mesiodistal dimension of the lesion was 17mm and superior-inferior dimension was 28mm.
The diagnosis of the OF was suggested based on the radiographic features of the lesion. The patient was referred to the Department of Maxillofacial and Oral Surgery and the lesion was surgically excised. Excisional biopsy confirmed the diagnosis of the OF.
3. Discussion
OF is a fibro-osseous lesion that is classified as a benign neoplasm which predominantly affects the jaws and facial bones. Owing to the presence of cementoid products in the OFs, these lesions were formerly considered as cemento-ossifying fibroma and cementifying fibroma [6]. However, it is now accepted that these terms are referred to as OF.
OF is generally slow-growing, asymptomatic and expansile lesion. The lesion tends to grow approximately equal in all directions, within the medullary part of the bone. This continuous growth of the lesion may result in the displacement of teeth or of the inferior alveolar canal and expansion of the outer cortical plates of bone although perforation and root resorption are rare [10].
In most cases, lesions are solitary, although a few cases of multiple occurrences have been reported [6]. Radiographically, OF may appear as a unilocular radiolucent lesion, a mixed-density or radiopaque lesion with a well-circumscribed, thinly corticated border [9,3,11]. The interior of the lesion depends on the duration of the lesion present. Early lesions are small and radiolucent. As they enlarge and mature, they present a mixed radiopaque radiolucent density and finally become completely radiopaque.
The most common method of managing OF is surgical excision[3]. Small and well-demarcated lesions can be treated by enucleation and curettage, whereas, lesions with rapid growth require radical resection with reconstruction [4]. Although the recurrence of this lesion reported to be rare, radiographic follow-up is required for assessing the recurrence after conservative surgical procedures [5].
Advanced imaging modalities such as CT or CBCT are usually performed to provide a more complete evaluation of the extent of the lesion and its internal structure. CBCT provides highly detailed sectional images of the osseous structures and teeth with a generally lower radiation dose compared to CT [12].
Here, in this report, a mixed-density expansile OF with a well-defined sclerotic border was visualized on the CBCT. Based on the three-dimensional radiographic images, it may be possible to distinguish the OF from fibrous dysplasia which usually blends into the surrounding bone unlike the well-defined OF that can be separated from the normal bone. The maturation stages of the OF are close to those of the cemento-osseous dysplasia which is predominantly small in size, and occurs mostly in anterior mandibular region of older patients. Additionally, the concentric expansion of the OF may help distinguish it from cemento-osseous dysplasia [6,10].
4. Conclusions
The diagnosis of the ossifying fibroma is made based on the clinical and radiological features of the lesion. The histology confirms the diagnosis.
References
- M. Glick, Burket’s Oral Medicine, 12th ed. Shelton (CT): PMPH-USA, 2015, ch. 7, p. 162.
- Eversole L.R., Leider A.S., Nelson K., Ossifying fibroma: a clinicopathologic study of sixty-four cases, Oral Surg. Oral Med. Oral Pathol. 60(5), 505-511 (1985).
- Liu Y., Wang H., You M., Yang Z., Miao J., Shimizutani K., Koseki T., Ossifying fibromas of the jaw bone: 20 cases, Dentomaxillofac. Radiol. 39(1), 57-63 (2010).
- Triantafillidou K., Venetis G., Karakinaris G., Iordanidis F., Ossifying fibroma of the jaws: a clinical study of 14 cases and review of the literature, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 114(2), 193-199 (2011).
- Titinchi F., Morkel J., Ossifying fibroma: analysis of treatment methods and recurrence patterns, J. Oral Maxillofac. Surg. 74(12), 2409-2419 (2016).
- MacDonald-Jankowski D.S., Fibro-osseous lesions of the face and jaws, Clin. Radiol. 59(1), 11-25 (2004).
- Eversole L.R., Merrell P.W., Strub D., Radiographic characteristics of central ossifying fibroma, Oral Surg. Oral Med. Oral Pathol. 59(5), 522-527 (1985).
- Trijolet J.P., Parmentier J., Sury F., Goga D., Mejean N., Laure B., Cemento-ossifying fibroma of the mandible, Eur. Ann. Otorhinolaryngol. Head Neck Dis. 128(1), 30-33 (2011).
- Araki M., Matsumoto K., Matsumoto N., Honda K., Ohki H., Komiyama K., Unusual radiographic appearance of ossifying fibroma in the left mandibular angle, Dentomaxillofac. Radiol. 39(5), 314-319 (2010).
- S.C. White and M.J. Pharoah, Oral Radiology: Principles and Interpretation, 7th ed. Missouri, USA: Mosby, 2004, ch. 22, pp. 394‑398.
- Shimamoto H., Kishino M., Okura M., Chindasombatjaroen J., Kakimoto N., Murakami S., Furukawa S., Radiographic features of a patient with both cemento-ossifying fibroma and keratocystic odontogenic tumor in the mandible: a case report and review of literature, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 112(6), 798-802 (2011).
- Loubele M., Maes F., Jacobs R., van Steenberghe D., White S.C., Suetens P., Comparative study of image quality for MSCT and CBCT scanners for dentomaxillofacial radiology applications, Radiat. Prot. Dosim. 129(1-3), 222-226 (2008).