Information
Journal Policies
Association of Hypothyroidism with Glaucoma: A Recent Update
Thekkuttuparambil Ananthanarayanan Ajith1*, Ranimenon2
2 Department of Ophthalmology, Dr Ranimenon’s eye clinic, Thrissur, Kerala, India
Copyright : © 2016 Thekkuttuparambil A A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The association of hypothyroidism with glaucoma is conflicting. Many population-based surveys showed an association of hypothyroidism including sub clinical hypothyroidism (SCH) with primary open angle glaucoma, while studies in some other population could not support such association. Though the conclusion about the role of thyroid hormone on ocular parameters is debatable, many studies reported that hypothyroidism could make changes in the interstitial connective tissue matrix, increased capillary density and increased serum lipid levels that may result in choroidal thickening. Hypothyroidism can increase the synthesis of glycosaminoglycans in the trabecular meshwork, result in a reduced aqueous outflow and, thereby, increased the intraocular pressure (IOP). An elevated IOP even in patients with SCH can lead to glaucoma. Furthermore, hypothyroidism increases the homocysteine level which will induce the death of retinal ganglion cells either by direct cytotoxic effect or mediated through oxidative stress. This review article discusses the possible association of hypothyroidism and glaucoma.
Keywords: Hypothyroidism; Open Angle Glaucoma; Intraocular Pressure; Orbitopathy; Thyroid-Stimulating Hormone; Choroidal Thickening, Glycosaminoglycans.
1.Introduction
Hypothyroidism, a decrease in thyroid hormone production by the thyroid gland and thereby lowered level in circulation can range from subclinical to overt hypothyroidism. Subclinical hypothyroidism (SCH) is characterised by serum thyroid hormone concentrations within the normal reference range with a single rise in serum thyroid-stimulating hormone (TSH) level. SCH is classified according to the serum TSH level into mild (increased TSH 4.0–10.0 mIU/L) and more severe categories where serum TSH concentrations increased to >10.0 mIU/L [1,2]. Canaris et al. reported the incidence of SCH varying between 4 and 10% depending on the gender, age and population studied [3].
Glaucoma is an important cause of blindness and the incidence of glaucoma was found to be increased over the age of 40 years [4]. Among the various etiological factors described a rise in intraocular pressure (IOP) and the associated optic disc damage remains the primary cause. A strong association of Graves' hyperthyroidism with orbitopathy with glaucoma has been reported with several plausible mechanisms [5,6]. Volume of orbital contents will increase that might cause orbital congestion and an associated increase in the episcleral venous pressure was suggested for the incidence of glaucoma [7]. Hypothyroidism had demonstrated as prevalent in glaucoma patients. Some studies demonstrated the association between hypothyroidism and glaucoma [8,9], while others failed to prove such association [10-13]. Smith et al. reported the prevalence of primary open angle glaucoma (POAG) in subjects with hypothyroidism which was as high as 23 %, while that of the control population was 4.7%. Furthermore, the same study demonstrated a decrease in IOP with the treatment of hypothyroidism in patient with glaucoma [8]. Centanni et al. also supported this with finding that the elevated IOP, even in patients with SCH at its early stages, could be reduced by treatment with levothyroxine [14]. Nevertheless, the screening for SCH in subjects with glaucoma has not yet been established. This review article discusses the association between hypothyroidism and glaucoma with the available literature.
2. Association of Hypothyroidism With Glaucoma
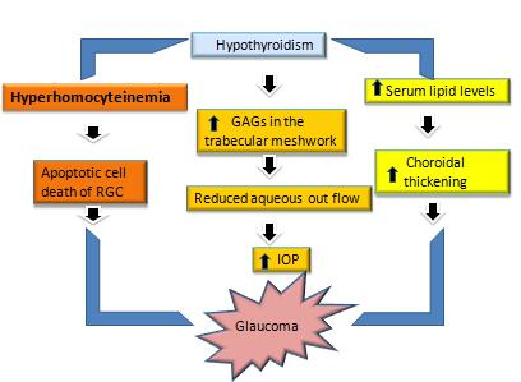
Thyroid hormones have a central role in the neural development of the eye mainly for the development of retina and attainment of color vision. They regulate mechanisms for controlling the cytoarchitecture and layering of retina. Various mechanisms were recommended to explain the link between glaucoma and hypothyroidism (Figure. 1). The IOP and body mass index were significantly higher in hypothyroid patients compared to healthy subjects [15]. Even in patients with subclinical and overt hypothyroidism, the IOP levels were significantly higher when compared to euthyroid patients and healthy subjects [16]. Smith et al. demonstrated that decreased thyroid hormone probably may increase the synthesis of glycosaminoglycans in the trabecular meshwork, result in a reduced aqueous outflow and, thereby, increased the IOP [17]. This was further supported in an autopsy study by Wittman that patients with hypothyroidism showed an increased interstitial connective tissue [18]. Hypothyroidism can make changes in the interstitial connective tissue matrix, increased capillary density and/or increased serum lipid levels that may result in choroidal thickening. Despite the role of thyroid hormone on IOP treatment with thyroxine showed multiple responses in ocular parameters in patients with hypothyroidism. A recent study in patients with overt hypothyroidism (without glaucoma) showed levothyroxine therapy normalised thyroid hormone levels without any change in the ocular parameters such as IOP, central corneal thickness (CCT), anterior chamber parameters, retinal nerve fiber layer thickness, retinal thickness and cup to disc ratio [16]. However, in euthyroid patients with levothyroxine treatment lowered the IOP level than patients with SCH and overt hypothyroidism [17]. Bahçeci et al. conducted an ophthalmic examination such as visual acuity, IOP, anterior segment and fundus examination together with computerized tomography and retinal nerve fiber layer thickness at the initial diagnosis and the third and ninth months of the L-thyroxine treatment [19]. They could find a reversible increase in the CCT leading to reversible IOP rise and thereby, decreased the CCT correlating with a decrease of TSH. Ozturk et al. reported that neither hypothyroidism, nor its replacement therapy gave rise to any change in IOP, CCT, anterior chamber parameters, retinal thickness and cup to disc ratio [15]. Hence, the conclusion on the role of thyroid hormone on the ocular parameters is debatable. Association of thyroid disorders has been reported in orbitopathy and glaucoma. Furthermore, the duration of active thyroid-associated orbitopathy is a marker of glaucomatous damage to the disc [7]. Morris et al. could demonstrate an association of hypothyroidism with hypercholesterolemia and hyperhomocysteinemia [20]. Hyperhomocysteinemia can explain the increased risk for glaucoma [21]. The mechanism can be either mediated through the direct cytotoxic effect of homocystein or the hmocysteine-induced oxidative stress [22,23]. Both of them lead to increased apoptotic death of retinal ganglion cells [24,25].
Figure1. Possible mechanism for hypothyroidism associated glaucoma. Hypothyroidism can increase the synthesis of glycosaminoglycans (GAGs) in the trabecular meshwork, result in a reduced aqueous outflow and, thereby, increased the IOP. An increase in the interstitial connective tissue matrix, serum lipid levels and increased capillary density may result in choroidal thickening. Furthermore, hypothyroidism increases the homocysteine level which will induce the death of retinal ganglion cells (RGC) either by direct cytotoxic effect or mediated through oxidative stress.
The consequences of SCH are variable at several levels and may depend on the duration and the degree of elevation of the serum TSH. Screening of thyroid function test revealed hypothyroidism in only 2.6% of POAG patients, whereas 4% in the control group [11]. A similar observation was found in a large case-control study conducted in the elderly population of US by Motsko and Jones, which demonstrated a prior hypothyroidism in 17.2% POAG patients and in 17.6% control subjects [13]. Ranimenon and Ajith had recently reported an incidence of SCH of 10.6% among the POAG patients at its early stages with female dominance [26]. However, the prevalence was not statistically significant when compared to the age and gender-matched healthy control subjects where the incidence of SCH was 14.4%. The population prevalence of SCH was approximately 5–10%, being more frequent in women and increasing prevalence with advancing age [3,27].
Population-based studies reported conflicting results. Recently Lin et al. during a 5-year follow-up period study in Taiwan population found that untreated hypothyroid patients had a significantly increased risk for POAG development [28] and levothyroxine was found to be protective [8,13,28]. A cross-sectional study was conducted in two large U.S. health survey in all subjects above the age of 40 years in order to know the association between hypothyroidism and glaucomatous. A total of 13,599 participants in National Health Interview Survey and 3,839 participants in National Health and Nutrition Examination Survey did not reveal any such association while considering univariate analysis [29]. A study by Tahat and al-Khawaldeh in 60 subjects of Jordan (age between 34-72 years) suggested a possible relationship between hypothyroidism and open-angle glaucoma [30]. A study from Greece by Karadimas et al. found no incidence of glaucoma in 100 newly diagnosed patients with hypothyroidism. Further claimed no correlation between IOP and either TSH or free tri-iodothyronine level [12]. A case-control study at Veterans Affairs Medical Center in Birmingham showed that subjects with a preexisting hypothyroidism have a greater risk of developing glaucoma than the healthy controls [31]. Therefore considering these reports, a large population-based study is warranted to establish the possibility of POAG in hypothyroid patients.
3. Conclusion and Future Perspectives
Though the association of hypothyroidism with glaucoma is debatable in various populations, the clinicians may screen for glaucoma in subjects with thyroid disorders especially in the presence of additional well-known risk factors for glaucoma. The thyroid function test at the early stage is beneficial for thyroxine therapy to prevent the worsening of glaucoma. While recommending for the thyroid hormone assay, a circadian fluctuation in serum TSH concentration need to be considered in both healthy individuals and those with SCH. The circadian fluctuation was observed mainly in the early afternoon and approximately 30% higher concentrations being present during the evening and night [32,33]. However, the degree of variation in serum TSH was lower in SCH when compared to other thyroid disorders like euthyroid. A further report found that in healthy individuals, TSH concentrations have a much smaller variation over time [34]. As a physiological adaptation to aging, a widening of the reference range for serum TSH with increasing age (>80 years old) should be considered [35,36]. Further, TSH levels correlate with obesity and markers of insulin resistance. Serum TSH concentrations >3.5 mU/L are commonly found in obesity [37]. Therefore, it may be recommended for repeat measurement of serum TSH, free thyroxine and antibodies against thyroid peroxidase, preferably after a 2- to 3-months interval in suspected cases [38]. Therefore, further critical prospective cohort studies are warranted to find the association between preexisting hypothyroidism and development of glaucoma.
References
- Duntas LH. Subclinical hypothyroidism: a misnomer in search of a new name. Thyroid 2001; 11: 361–362.
- Gharib H, Tuttle RM, Baskin HJ, Fish LH, Singer PA, McDermott MT. Subclinical thyroid dysfunction: a joint statement on management from the American Association of Clinical Endocrinologists, the American Thyroid Association, and the Endocrine Society. J Clin Endocrinol Metab 2005; 90: 581–585.
- Canaris GJ, Manowitz NR, Mayor G, Ridgway EC: The Colorado thyroid disease prevalence study. Arch Intern Med 2000; 160: 526–534.
- Coleman AL, Miglior S. Risc factors for glaucoma onset and progression. Surv Ophthalmol. 2008; 53(Supll 1):3-10.
- Bhat S, Unnikrishnan AG, Jeyapathy P, Kumar H, Jayakumar RV. Glaucoma and thyroid disease-An interesting association. Thyroid Res Pract 2010;7:35-6.
- Putta-Manohar S, Perros P. Epidemiology of Graves' orbitopathy. Pediatr Endocrinol Rev 2010;7:S182-5.
- Cockerham KP, Pal C, Jani B, Wolter A, Kennerdell JS. The prevalence and implications of ocular hypertension and glaucoma in thyroid-associated orbitopathy. Ophthalmology 1997;104:914-7.
- Smith KD, Arthurs BP, Saheb N. An association between hypothyroidism and primary open-angle glaucoma. Ophthalmol 1993;100:1580-4.
- Cross JM, Girkin CA, Owsley C, McGwin G Jr. The association between thyroid problems and glaucoma. Br J Ophthalmol 2008;92:1503-5.
- Kitsos G, Pappa C, Tsatsoulis A. Primary open angle glaucoma and hypothyroidism. J Clin Optom 2010;2:5-8.
- Muñoz-Negrete FJ, Rebolleda G, Almodóvar F, Díaz B, Varela C. Hypothyroidism and primary open-Aangle glaucoma. Ophthalmologica 2000;214:347–349.
- Karadimas, P, Bouzas EA, Topouzis F, Koutras DA, Mastorakos G, Hypothyroidism and glaucoma. A study of 100 hypothyroid patients. Am J Ophthalmol. 2001;131: 126-128.
- Motsko SP, Jones, JK. Is There an Association between Hypothyroidism and Open-angle Glaucoma in an Elderly Population? An Epidemiologic Study. Ophthalmology 2008;115:1581-4.
- Centanni M, Cesareo R, Verallo O, Brinelli M, Canettieri G, Viceconti N, et al. Reversible increase of intraocular pressure in subclinical hypothyroid patients. Eur J Endocrinol 1997;136:595-8.
- Ozturk BT, Kerimoglu H, Dikbas O, Pekel H, Gonen MS. Ocular changes in primary hypothyroidism. BMC Res Notes 2009;2:266.
- Ulas F, Dogan U, Dikbas O, Çelebi S, Keles A. Investigation of the choroidal thickness in patients with hypothyroidism. Indian J Ophthalmol. 2015: 63: 244-249.
- Smith TJ, Murata Y, Horwitz AL, Philipson L, Refetoff S. Regulation of glycosaminoglycan synthesis by thyroid hormone in vitro. J Clin Invest 1982;70:1066-73.
- Wittmann AL. Macroglossia in acromegaly and hypothyroidism. Virchows Arch A Pathol Anat Histol 1977;373:353-60.
- Bahçeci UA, Özdek Ş, Pehlivanlı Z, Yetkin İ, Önol M. Changes in intraocular pressure and corneal and retinal nerve fiber layer thicknesses in hypothyroidism. Eur J Ophthalmol 2005; 15:556-61.
- Morris MS, Bostom AG, Jacques PF, Selhub J, Rosenberg IH. Hyperhomocysteinemia and hypercholesterolemia associated with hypothyroidism in the third US National Health and Nutrition Examination Survey. Atherosclerosis. 2001;155:195-200.
- Wang G, Medeiros FA, Barshop BA, Weinreb RN. Total plasma homocysteine and primary open-angle glaucoma. Am J Ophthalmol 2004, 137:401-406.
- Feldman F, Sweeney V, Drance S. Cerebro-vascular studies in chronic simple glaucoma. Can J Ophthalmol. 1969;4:358–364.
- Wagenfeld L, Weiss S, Klemm M, Richard G, Zeitz O. Vascular dysfunction in ocular blood flow regulation: impact of reactive oxygen species in an experimental setup. Invest Ophthalmol Vis Sci. 2014;55:5531-5536.
- Ajith TA,Ranimenon. Homocysteine in ocular diseases. Clin Chim Acta. 2015; 23:450:316-21.
- Moore P, El-Sherbeny A, Roon P Schoenlein PV, Ganapathy V, Smith SB. Apoptotic cell death in the mouse retinal ganglion cell layer is induced in vivo by the excitatory amino acid homocysteine. Exp Eye Res. 2001;73:45–57.
- Ranimenon, Ajith TA. Prevalence of hypothyroidism in glaucoma patients. Kerala J Ophthalmol. 2015;27:196-200.
- Vanderpump MP, Tunbridge WM. Epidemiology and prevention of clinical and subclinical hypothyroidism. Thyroid 2002; 12: 839–847.
- Lin HC, Kang JH, Jiang YD, Ho JD. Hypothyroidism and the risk of developing open-angle glaucoma: A five-year population-based follow-up study. Ophthalmology 2010;117:1960-6.
- Kakigi C, Kasuga T, Wang SY, Singh K, Hiratsuka Y, Murakami A, Lin SC. Hypothyroidism and Glaucoma in The United States. PLoS One. 2015;10:e0133688.
- Tahat AA, al-Khawaldeh AM. Hypothyroidism and open-angle glaucoma: an accidental or an essential coexistence? East Mediterr Health J. 2000;6:299-303.
- Girkin CA, McGwin G Jr, McNeal SF, Lee PP, Owsley C. Hypothyroidism and the development of open-angle glaucoma in a male population. Ophthalmology. 2004;111:1649-52.
- Roelfsema F, Pereira AM, Veldhuis JD, Adriaanse R, Endert E, Fliers E, et al. Thyrotropin secretion profiles are not differentin men and women. J Clin Endocrinol Metab 2009; 94: 3964– 3967.
- Roelfsema F, Pereira AM, Veldhuis JD, Adriaanse R, Endert E, Fliers E, et al. Thyrotropin secretion in mild and severe primary hypothyroidism is distinguished by amplified burst mass and basal secretion with increased spikiness and approximate entropy. J Clin Endocrinol Metab 2010; 95: 928–934.
- Andersen S, Pedersen KM, Bruun NH, Laurberg P. Narrow individual variations in serum T 4 and T 3 in normal subjects: a clue to the understanding of subclinical thyroid disease. J Clin Endocrinol Metab 2002; 87: 1068–1072.
- Surks MI, Hollowell JG: Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J Clin Endocrinol Metab 2007; 92: 4575–4582.
- Atzmon G, Barzilai N, Hollowell JG, Barzilai N, Hollowell JG, Surks MI, et al. Extreme longevity is associated with increased serum thyrotropin. J Clin Endocrinol Metab 2009; 94: 1251–1254.
- Asvold BO, Bjoto T, Vatten LJ. Association of serum TSH with high body mass differs between smokers and never-smokers. J Clin Endocrinol Metab 2009; 94: 5023–5027.
- Pearce SHS, Brabant G, Duntas LH, Monzani F, Peeters RP, Razvi S, et al. 2013 ETA guideline: Management of subclinical hypothyroidism. Eur Thyroid J. 2013;2:215–228.